Crohn’s disease is a chronic inflammatory bowel disease (IBD) that affects various parts of the gastrointestinal (GI) tract, from the mouth to the anus. It can cause serious complications and significantly impact an individual’s quality of life. The inflammation caused by Crohn’s can penetrate deep into the layers of affected bowel tissue, leading to painful and often debilitating symptoms. This condition requires long-term treatment and careful management to maintain a good quality of life.
In this in-depth guide, we will explore the symptoms, causes, and effective treatment options for Crohn’s disease. Our goal is to help readers gain a comprehensive understanding of this complex condition and provide guidance on how to manage it effectively.
Table of Contents
What Is Crohn’s Disease?
Crohn’s infection has a place with a gathering of conditions known as provocative inside sicknesses (IBD). Not at all like ulcerative colitis, which influences just the colon, Crohn’s infection can influence any piece of the GI lot, however it most generally influences the ileum (the lower end of the small digestive system) and the start of the colon.
This disease is characterized by periods of remission (when symptoms improve or disappear) and flare-ups (when symptoms worsen). Crohn’s disease is not curable, but with the right combination of treatment and lifestyle modifications, many people can manage their symptoms and lead fulfilling lives.
Detailed Symptoms of Crohn’s Disease
The side effects of Crohn’s infection can fluctuate broadly contingent upon the area and seriousness of the aggravation. Some people experience mild symptoms, while others have more severe and chronic issues. Here’s a deeper look at the symptoms:
1. Chronic Diarrhea
One of the most common symptoms of Crohn’s disease is chronic diarrhea, which may last for weeks or months. The inflammation in the intestines can lead to an increase in bowel movements, often with an urgent need to use the bathroom. The diarrhea may contain mucus, blood, or pus, depending on the severity of the disease.
Managing Chronic Diarrhea: Doctors often prescribe antidiarrheal medications, but it is crucial to treat the underlying inflammation to prevent long-term damage to the intestines. Additionally, hydration is critical to prevent dehydration caused by excessive fluid loss.
2. Abdominal Pain and Cramping
Patients with Crohn’s often experience severe abdominal pain. This pain typically occurs in the lower right part of the abdomen, but it can occur anywhere depending on the location of the inflammation.
Pain Patterns: The pain is usually described as cramping, and it can worsen after eating, as the digestive system is active. The inflammation, ulcers, and scarring in the intestines can lead to obstructions, which may cause extreme discomfort.
3. Blood in Stool
When the lining of the digestive tract is inflamed, it can bleed. Blood in the stool is often a sign of severe inflammation, ulcers, or tears in the bowel wall. This symptom can be alarming for many patients and may indicate a need for immediate medical attention.
- Blood Appearance: The blood may appear bright red (indicating it is from the lower part of the GI tract) or dark and tarry (indicating bleeding from higher up).
4. Fatigue and Weakness
Fatigue is a frequent issue for Crohn’s patients. Chronic inflammation, frequent bowel movements, malnutrition, and dehydration can lead to a feeling of constant tiredness and weakness.
5. Unintentional Weight Loss
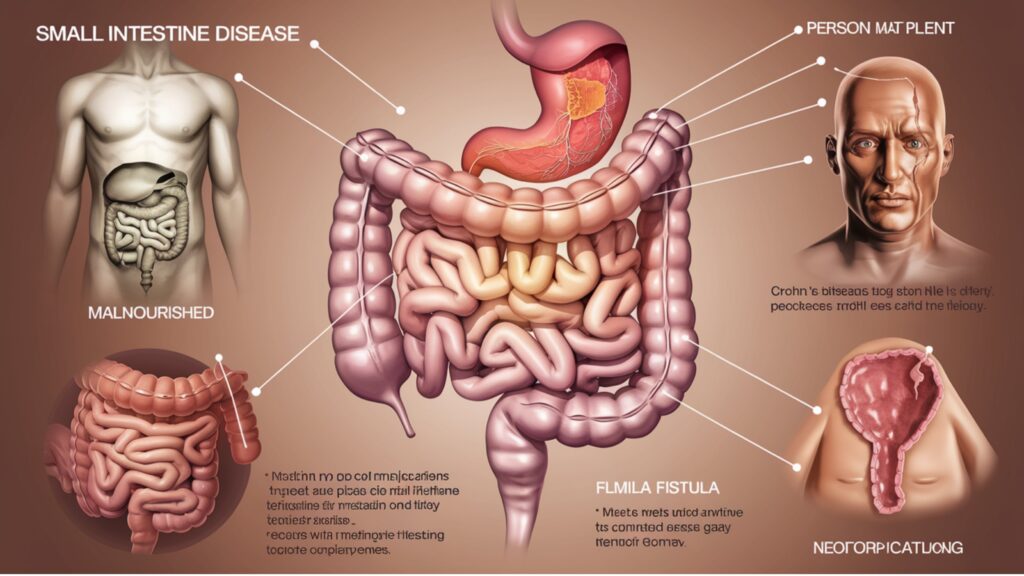
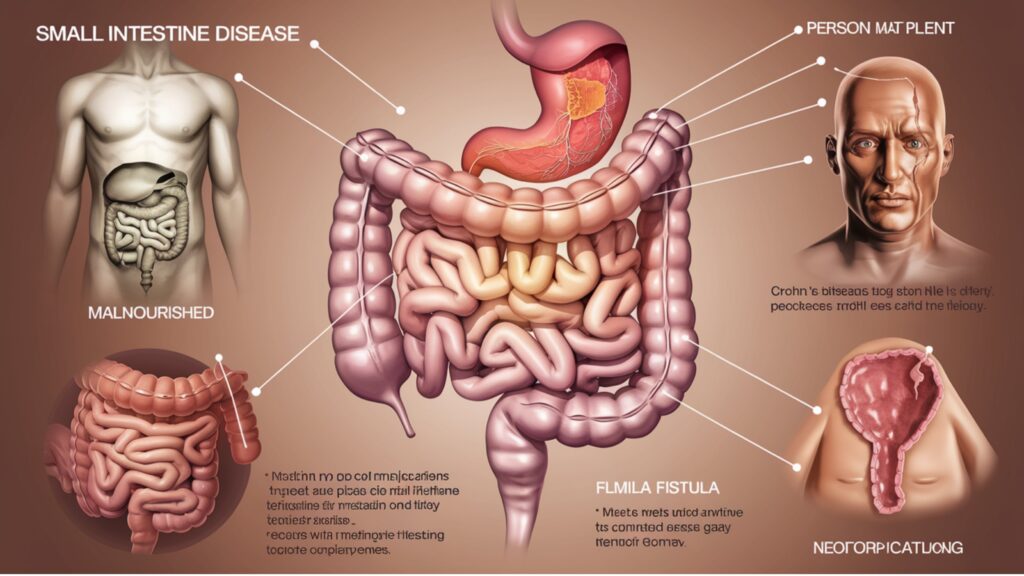
Because Crohn’s disease affects the body’s ability to absorb nutrients, many patients experience unintentional weight loss. Inflammation in the small intestine can impair digestion and the absorption of essential nutrients like fats, proteins, and carbohydrates.
- Nutrient Deficiency: This leads to malnutrition, and patients may need to follow a specific diet or take supplements to ensure they get enough nutrients.
6. Fistulas
A fistula is a strange association between two pieces of the body. In Crohn’s disease, fistulas can form between different parts of the intestine or between the intestine and other organs such as the bladder or skin.
- Complications: Fistulas can be incredibly painful and may require surgery to repair.
7. Reduced Appetite and Nausea
The inflammation in the GI tract often causes nausea, leading to a reduced appetite. Over time, patients may avoid food to prevent the pain and discomfort that can follow meals, which further contributes to weight loss and malnutrition.
Causes of Crohn’s Disease
The exact cause of Crohn’s disease is still unknown, but a combination of factors may contribute to its development. Researchers believe that genetics, the immune system, and environmental factors all play a role. We should investigate these causes.
1. Genetic Factors
People with a family history of Crohn’s disease or other IBDs are more likely to develop the condition. Several genes, including NOD2, have been identified as contributing to the development of Crohn’s disease. These genes affect the body’s immune response and the function of the intestinal barrier.
- Family History: Studies have shown that people with a first-degree relative with Crohn’s disease are more likely to develop it themselves, suggesting a strong genetic component.
2. Immune System Dysfunction
In people with Crohn’s disease, the immune system mistakenly attacks the healthy cells of the digestive tract. This abnormal immune response leads to chronic inflammation and damage to the intestinal walls.
- Autoimmune Response: The body’s immune system, which is supposed to fight off harmful invaders, ends up attacking its own tissues. This results in the inflammation that characterizes Crohn’s disease.
3. Environmental Triggers
Several environmental factors may act as triggers for Crohn’s disease or exacerbate its symptoms.
- Diet: Diets high in refined sugars, fats, and processed foods have been linked to an increased risk of Crohn’s disease. Although no single food is known to cause Crohn’s disease, some dietary patterns may trigger flare-ups.
- Smoking: Smoking is a significant risk factor. Smokers are more likely to develop Crohn’s disease, and their symptoms are often more severe.
- Infections: Some researchers believe that bacterial or viral infections may play a role in triggering the abnormal immune response seen in Crohn’s disease.
4. Age and Geography
Crohn’s disease can occur at any age, but it is most often diagnosed in individuals between 15 and 35 years old. Geographically, it is more common in industrialized countries and in urban areas, suggesting that environmental factors such as diet, hygiene, and access to healthcare may influence its development.
Effective Treatment Options for Crohn’s Disease
There is no cure for Crohn’s disease, but several treatments can help manage the symptoms and reduce inflammation. The goal of treatment is to induce and maintain remission, reduce flare-ups, and improve quality of life.
1. Medications
Several types of medications are commonly used to treat Crohn’s disease:
a. Anti-inflammatory Drugs
The first step in treating Crohn’s disease is to reduce the inflammation that causes symptoms. Common anti-inflammatory medications include:
- Corticosteroids: These are used for short-term relief during flare-ups to reduce inflammation rapidly. However, long-term use is not recommended due to potential side effects such as weight gain, osteoporosis, and increased risk of infections.
- Aminosalicylates: These are used for long-term management and are effective in reducing inflammation in the GI tract.
b. Immunosuppressants
Medications such as azathioprine and methotrexate suppress the immune system’s abnormal response. These drugs are often used when patients do not respond to anti-inflammatory medications alone.
c. Biologic Therapies
Biologics like infliximab and adalimumab target specific proteins in the immune system to reduce inflammation. These medications are typically used for moderate to severe Crohn’s disease.
d. Antibiotics
Antibiotics such as metronidazole and ciprofloxacin are sometimes used to treat infections and fistulas in Crohn’s disease patients.
2. Dietary Management
Dietary changes play a critical role in managing Crohn’s disease. While no specific diet works for everyone, there are general recommendations to help control symptoms:
a. Low-Residue Diet
A low-residue diet minimizes high-fiber foods to reduce the frequency of bowel movements. This can help manage diarrhea and abdominal pain.
b. Hydration and Nutritional Support
Crohn’s patients often struggle with malnutrition due to poor nutrient absorption. Supplements or specialized nutrition plans are sometimes necessary to ensure the patient gets adequate vitamins and minerals.
c. Elimination Diet
Some patients find relief by eliminating foods that trigger symptoms. Working with a dietitian can help identify these triggers.
3. Surgical Interventions
For some patients, surgery becomes necessary when medications no longer work, or complications like fistulas, abscesses, or obstructions occur. Surgical options include:
a. Resection
Resection involves removing the diseased portion of the intestine and reconnecting the healthy parts. This procedure can relieve symptoms but does not cure the disease, as inflammation can recur in other areas.
b. Strictureplasty
In this surgery, the narrowed portions of the intestine are widened without removing any part of the bowel.
c. Colostomy or Ileostomy
In cases where large portions of the intestine need to be removed due to severe damage or complications from Crohn’s disease, a surgeon may create a stoma, which is an artificial opening through the abdominal wall. Waste is diverted through this opening into a bag outside the body. While it is a life-altering procedure, it can significantly improve the quality of life for those with severe Crohn’s disease who suffer from frequent obstructions, fistulas, or abscesses.
- When Surgery is Necessary: Surgery is generally considered a last resort when other treatments have failed or when complications like intestinal blockages, fistulas, or perforations develop. Up to 70% of people with Crohn’s disease will require some form of surgery during their lifetime. Despite this, surgery does not cure Crohn’s, and many patients may still need ongoing medical treatment to manage the disease after surgery.
Preventing Flare-Ups and Long-Term Management
Crohn’s disease requires continuous management to prevent flare-ups and complications. Here are key strategies for preventing flare-ups and living a healthier life with Crohn’s:


1. Follow a Customized Diet Plan
Working with a nutritionist or dietitian to develop a personalized diet plan is crucial for long-term management. Avoiding known trigger foods and following a diet that minimizes inflammation can make a big difference in how often flare-ups occur.
Key Dietary Tips:
- Stick to small, frequent meals to ease digestion.
- Limit high-fiber foods (especially during flare-ups) to avoid irritating the bowel.
- Stay hydrated by drinking plenty of water to counter the effects of diarrhea and avoid dehydration.
- Keep a food diary to track which foods may trigger flare-ups.
2. Quit Smoking
Smoking not only increases the risk of developing Crohn’s disease but also makes symptoms worse for those already diagnosed. Quitting smoking is one of the most important lifestyle changes that can lead to fewer flare-ups and slower disease progression.
3. Manage Stress
While stress does not directly cause Crohn’s disease, it can exacerbate symptoms and trigger flare-ups. Managing stress through relaxation techniques such as meditation, yoga, and deep-breathing exercises can help improve overall well-being.
4. Regular Medical Check-Ups
Routine visits to a gastroenterologist are essential for monitoring disease progression, adjusting treatments, and identifying potential complications early. Blood tests, colonoscopies, and imaging studies like MRIs and CT scans are commonly used to evaluate the condition of the intestines.
5. Take Medications as Prescribed
Consistency in taking prescribed medications can help maintain remission and prevent flare-ups. Patients should follow their doctors’ recommendations closely and notify them if side effects occur or if symptoms worsen.
6. Exercise Regularly
Moderate physical activity can help reduce stress, improve mood, and aid digestion. Exercise like walking, swimming, or yoga is generally safe for most Crohn’s patients. However, during active flare-ups, it may be necessary to modify physical activity to avoid discomfort.
Potential Complications of Crohn’s Disease
If left untreated or poorly managed, Crohn’s disease can lead to a range of serious complications, some of which may require immediate medical intervention. It’s important to recognize these complications to prevent long-term damage to the intestines and other organs.
1. Bowel Obstruction
Chronic inflammation from Crohn’s disease can cause sections of the intestine to thicken and scar over time. This scarring can narrow the intestine, leading to a bowel obstruction, where food or stool is unable to pass through. Symptoms of a bowel obstruction include severe abdominal pain, vomiting, and bloating. Surgery is often required to remove the blocked portion of the bowel.
2. Ulcers
Crohn’s disease can cause open sores (ulcers) anywhere along the GI tract, including the mouth, anus, and even genital area. These ulcers can become deep and may lead to further complications, such as infections.
3. Fistulas
As mentioned earlier, fistulas are abnormal connections that can form between the intestines and other parts of the body, such as the bladder, vagina, or skin. Fistulas can become infected and cause abscesses, which may require surgical treatment.
4. Malnutrition
The inflammation caused by Crohn’s can interfere with the body’s ability to absorb nutrients, leading to malnutrition. This can result in deficiencies in essential vitamins and minerals, which can weaken bones (osteoporosis), impair the immune system, and cause general fatigue and weakness. Nutritional supplementation, either through diet or intravenous solutions, is sometimes necessary.
5. Colorectal Cancer
Patients with Crohn’s disease, particularly those with long-standing inflammation of the colon, are at an increased risk for developing colorectal cancer. Regular screenings, including colonoscopies, are critical for detecting precancerous changes early and reducing the risk of cancer.
6. Perianal Disease
Crohn’s disease can affect the area around the anus, causing complications like abscesses and fistulas. These painful conditions can lead to infection and often require medical or surgical intervention to manage.
Future Outlook for Crohn’s Disease Treatment
Ongoing research into the causes and treatment of Crohn’s disease holds promise for future advancements. New therapies and medications are being developed, and researchers are working on ways to personalize treatment for each individual based on their genetic makeup, immune response, and environmental factors.


1. Stem Cell Therapy
Stem cell therapy is one of the most exciting areas of research for Crohn’s disease. Early trials have shown that stem cells may help repair damaged tissues in the intestines, offering hope for long-term remission.
2. Personalized Medicine
As scientists learn more about the genetic and environmental factors that contribute to Crohn’s disease, there is hope that future treatments can be tailored to individual patients. Personalized medicine could lead to more effective treatment plans that are designed based on a patient’s specific genetic profile and immune system activity.
3. New Biologic Therapies
Biologic therapies that target specific components of the immune system are continually being refined. These therapies have the potential to reduce inflammation more effectively and with fewer side effects than traditional immunosuppressants. New biologic drugs are being tested in clinical trials and may soon offer additional treatment options for patients with moderate to severe Crohn’s disease.
Living with Crohn’s Disease
Living with Crohn’s disease can be challenging, but with proper medical care, lifestyle adjustments, and support, many people manage to lead active and fulfilling lives. Awareness of symptoms, regular medical check-ups, and adherence to treatment plans are key to keeping the disease under control.
Final Thoughts
Crohn’s disease is a chronic and complex condition, but understanding its symptoms, causes, and treatment options can empower individuals to take control of their health. While there is currently no cure for Crohn’s disease, modern treatments—ranging from medications to surgeries and lifestyle changes—have significantly improved the quality of life for many patients. As research continues, the future holds even more promise for those living with Crohn’s disease.
Whether you’re newly diagnosed or have been managing Crohn’s for years, staying informed and proactive in your treatment is the best way to manage this condition. With ongoing advancements in treatment, there is always hope for improved health and wellness.
FAQs
What causes Crohn’s disease?
The specific reason for Crohn’s infection isn’t completely perceived. In any case, it is accepted to result from a blend of hereditary, ecological, and resistant framework factors. In people with Crohn’s disease, the immune system mistakenly attacks healthy tissue in the gastrointestinal (GI) tract, leading to inflammation.
Is Crohn’s disease curable?
There is currently no cure for Crohn’s disease. However, with proper medical treatment, lifestyle changes, and dietary management, many individuals are able to achieve remission, where symptoms are greatly reduced or disappear for periods of time.
What are common symptoms of Crohn’s disease?
Common symptoms include persistent diarrhea, abdominal pain, cramping, fatigue, weight loss, and sometimes blood in the stool. These symptoms can vary in severity and can come and go during periods of flare-ups and remission.
What is the contrast between Crohn’s illness and ulcerative colitis?
Both Crohn’s disease and ulcerative colitis are types of inflammatory bowel disease (IBD). The key difference is that Crohn’s disease can affect any part of the GI tract from the mouth to the anus, whereas ulcerative colitis is limited to the colon and rectum. Additionally, Crohn’s disease affects all layers of the intestinal wall, while ulcerative colitis only affects the innermost lining of the colon.
Can diet affect Crohn’s disease symptoms?
Yes, diet plays a significant role in managing Crohn’s disease. While specific trigger foods can vary from person to person, many individuals find that avoiding certain foods, such as spicy foods, dairy, and high-fiber items, can help reduce symptoms during flare-ups. It is important to work with a healthcare provider or dietitian to develop a personalized diet plan.