Congestive heart failure (CHF) is a serious medical condition affecting millions of people worldwide, particularly in the United States. It occurs when the heart is unable to pump blood efficiently to meet the body’s needs, leading to fluid buildup in various parts of the body such as the lungs, legs, and abdomen. This condition is chronic, and while it can’t be cured, there are numerous treatment options available that can help manage symptoms and improve quality of life. In this blog post, we will explore the symptoms, causes, and treatment options for congestive heart failure, providing a comprehensive guide for anyone looking to understand this condition better.
Table of Contents
What is Congestive Heart Failure?
Congestive heart failure is a form of heart failure that results in the accumulation of fluid in the body’s tissues. It can occur on either side of the heart—left-sided or right-sided heart failure—or both. In left-sided heart failure, fluid builds up in the lungs, causing shortness of breath. Right-sided heart failure causes fluid to accumulate in the abdomen, legs, and feet, leading to swelling.
While “heart failure” may sound like the heart has completely stopped working, that’s not the case. It implies that the heart’s siphoning power is more fragile than ordinary. As the heart struggles to supply the body’s cells with adequate blood and oxygen, fluid builds up in the tissues, causing various symptoms and complications.
Symptoms of Congestive Heart Failure
Recognizing the symptoms of congestive heart failure is crucial for early diagnosis and treatment. The symptoms can vary depending on the severity of the condition, but common indicators include:


- Shortness of Breath: This is one of the hallmark symptoms of congestive heart failure. It often occurs during physical activity, but it can also manifest when you’re lying down. This happens because the weakened heart allows fluid to accumulate in the lungs, causing difficulty breathing.
- Fatigue and Weakness: People with CHF often experience constant fatigue due to the heart’s inability to pump enough blood to meet the body’s energy needs. As a result, routine tasks can feel exhausting.
- Swelling (Edema): Fluid retention is a major symptom of congestive heart failure. You may notice swelling in your legs, ankles, feet, or abdomen, caused by fluid buildup in the tissues.
- Rapid or Irregular Heartbeat: CHF can cause your heart to beat faster to compensate for its reduced pumping efficiency. You may also experience palpitations or arrhythmias (irregular heartbeats).
- Persistent Cough or Wheezing: A chronic cough, especially one that produces white or pink, blood-tinged mucus, can be a sign that fluid is accumulating in the lungs due to congestive heart failure.
- Increased Need to Urinate at Night: Congestive heart failure may cause a need to urinate more frequently at night (nocturia) as the body tries to expel excess fluid.
- Sudden Weight Gain: Rapid weight gain is often a sign of fluid retention. If you gain more than 2-3 pounds in a day or 5 pounds in a week, it may be a sign that your heart failure is worsening.
- Lack of Appetite and Nausea: CHF can interfere with digestion, causing a loss of appetite, nausea, or a feeling of fullness due to fluid buildup around the liver and intestines.
Causes of Congestive Heart Failure
There are many conditions that can lead to congestive heart failure, either by damaging the heart muscle or by making it work harder than normal. Below are the most common causes of congestive heart failure:
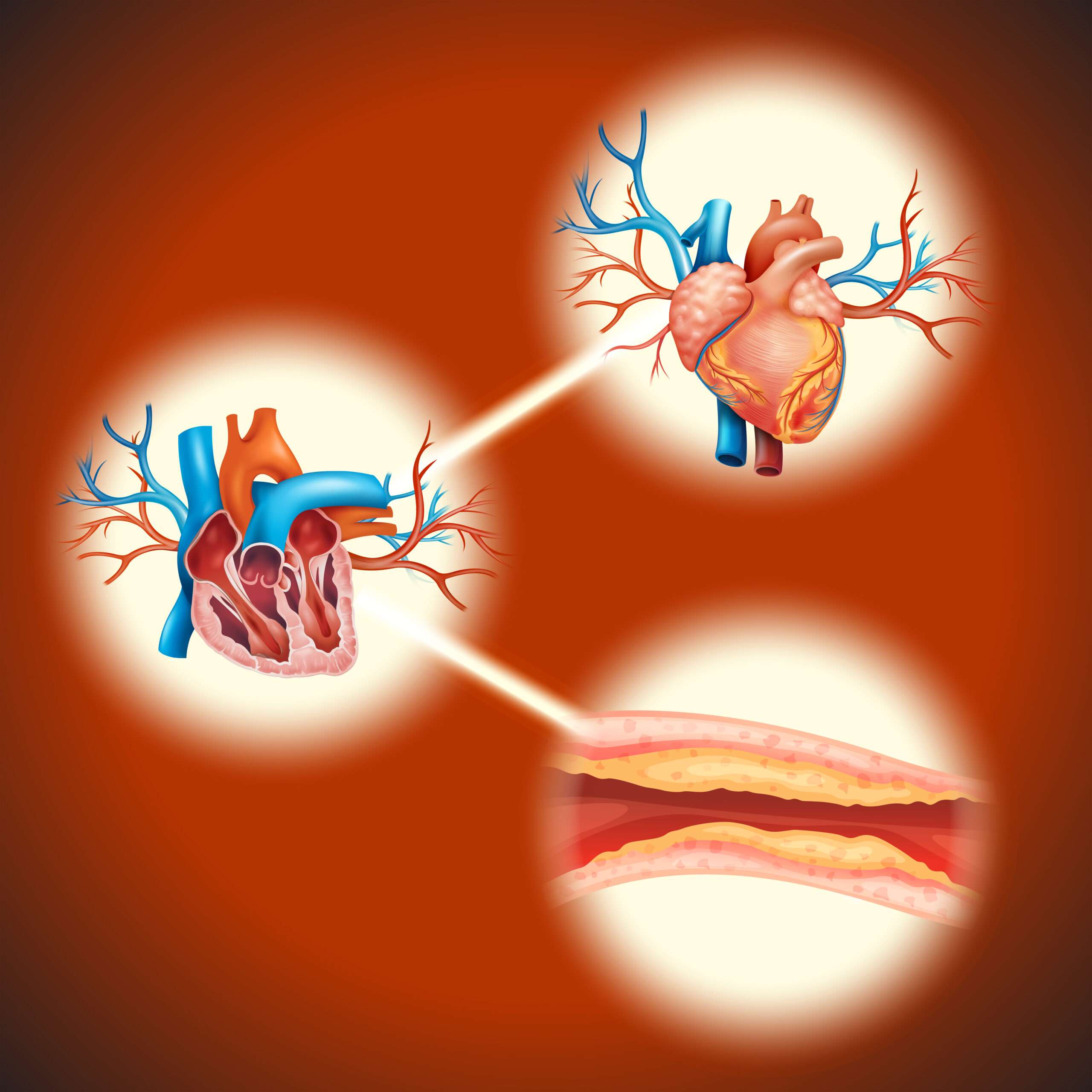
1. Coronary Artery Disease (CAD)
Coronary artery disease is one of the leading causes of congestive heart failure. CAD occurs when the arteries that supply blood to the heart become narrowed or blocked due to plaque buildup, reducing blood flow to the heart muscle. Over time, this can weaken the heart and lead to heart failure.
2. High Blood Pressure (Hypertension)
Chronic high blood pressure forces the heart to work harder than normal to pump blood throughout the body. Over time, this increased workload can lead to the thickening of the heart muscle and, eventually, congestive heart failure.
3. Heart Attack
A heart attack occurs when blood flow to a part of the heart is blocked, damaging or killing heart tissue. This can weaken the heart’s ability to pump blood, leading to heart failure. The more severe the heart attack, the greater the risk of developing congestive heart failure.
4. Cardiomyopathy
Cardiomyopathy alludes to illnesses of the heart muscle that make it become amplified, thick, or unbending. This can impair the heart’s ability to pump blood effectively, eventually leading to heart failure. Cardiomyopathy can be caused by genetic factors, infections, alcohol abuse, and certain medications.
5. Valvular Heart Disease
Heart valves regulate blood flow through the heart’s chambers. When these valves become damaged or dysfunctional—whether due to infection, aging, or a congenital defect—the heart has to work harder to pump blood, increasing the risk of heart failure.
6. Diabetes
Diabetes increases the risk of congestive heart failure by contributing to high blood pressure, coronary artery disease, and other heart conditions. Poorly managed blood sugar levels can damage blood vessels and nerves, including those controlling the heart.
7. Obesity
Obesity puts extra strain on the heart and increases the risk of conditions that can lead to heart failure, such as high blood pressure, diabetes, and coronary artery disease.
8. Other Contributing Factors
In addition to the primary causes listed above, several other factors can contribute to congestive heart failure. These include:
- Chronic kidney disease
- Thyroid disorders
- Sleep apnea
- Severe infections (e.g., sepsis)
- Excessive alcohol consumption
Types of Congestive Heart Failure
Congestive heart failure can be classified into different types based on which part of the heart is affected and how the heart’s function is impaired.
1. Left-Sided Heart Failure
This is the most widely recognized type of cardiovascular breakdown. It occurs when the left ventricle (the heart’s main pumping chamber) is unable to pump blood efficiently. Left-sided heart failure can be further divided into:
- Systolic Cardiovascular breakdown: The passed on ventricle loses its capacity to contract regularly, decreasing how much blood that is siphoned out with every heartbeat.
- Diastolic Heart Failure: The left ventricle becomes stiff and unable to relax properly, preventing the heart from filling with enough blood between beats.
2. Right-Sided Heart Failure
Right-sided cardiovascular breakdown happens when the right ventricle neglects to siphon blood really to the lungs. This leads to fluid buildup in the abdomen, legs, and feet. Right-sided heart failure is often caused by left-sided heart failure, as increased pressure in the lungs puts strain on the right side of the heart.
3. Congestive Heart Failure with Preserved Ejection Fraction (HFpEF)
This form of heart failure occurs when the heart’s pumping function remains normal, but the heart is still unable to meet the body’s needs due to issues with relaxation and filling. HFpEF is more common in older adults, women, and people with high blood pressure.
Diagnosis of Congestive Heart Failure
Diagnosing congestive heart failure typically involves a combination of medical history, physical exams, and diagnostic tests. Key tests for diagnosing CHF include:8
- Echocardiogram: This ultrasound test creates images of the heart’s structure and function, allowing doctors to assess the heart’s ability to pump blood.
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect arrhythmias or signs of previous heart attacks.
- Chest X-Ray: A chest X-ray can reveal fluid buildup in the lungs and other signs of heart failure, such as an enlarged heart.
- Blood Tests: Blood tests can help identify underlying conditions that contribute to heart failure, such as high cholesterol, diabetes, or kidney disease. A specific blood test for a substance called B-type natriuretic peptide (BNP) is often used to diagnose and assess the severity of heart failure.
- Stress Test: A stress test measures how well your heart performs under physical stress (e.g., during exercise). It can help assess the severity of heart failure and guide treatment decisions.
Treatment Options for Congestive Heart Failure
While congestive heart failure is a chronic condition, there are numerous treatment options that can help manage symptoms, slow disease progression, and improve quality of life. Treatment for CHF often involves a combination of medications, lifestyle changes, and, in some cases, surgery or medical devices.
1. Medications
Medications are the cornerstone of treatment for congestive heart failure. Commonly prescribed medications include:
- ACE Inhibitors: These drugs relax blood vessels and reduce blood pressure, easing the workload on the heart. Examples include lisinopril and enalapril.
- Beta-Blockers: Beta-blockers reduce heart rate and lower blood pressure, improving heart function and reducing the risk of further heart damage. Examples include metoprolol and carvedilol.
- Diuretics: Also known as “water pills,” diuretics help remove excess fluid from the body, reducing swelling and relieving shortness of breath. Common diuretics include furosemide and spironolactone.
- Aldosterone Antagonists: These medications block the effects of a hormone called aldosterone, which can worsen heart failure. Examples include spironolactone and eplerenone.
- Digoxin: This medication helps the heart pump more efficiently and can help control irregular heartbeats, particularly in patients with atrial fibrillation.
- ARNIs (Angiotensin Receptor-Neprilysin Inhibitors): This newer class of medication, including drugs like sacubitril/valsartan (Entresto), combines a neprilysin inhibitor and an angiotensin receptor blocker (ARB) to reduce strain on the heart and improve outcomes in patients with heart failure.
2. Lifestyle Changes
Lifestyle modifications are critical in managing congestive heart failure. Here are some of the most effective changes that can improve symptoms and slow the progression of the disease:
- Dietary Changes: A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) or Mediterranean diet, can help reduce the strain on your heart. Limiting sodium intake to less than 2,000 mg per day is crucial for reducing fluid retention. Focus on eating fresh fruits, vegetables, whole grains, lean proteins, and healthy fats, while avoiding processed and high-sodium foods.
- Fluid Management: Since congestive heart failure often leads to fluid buildup, it’s essential to monitor and limit your fluid intake. Your doctor may recommend a specific daily fluid limit to prevent worsening symptoms.
- Exercise: While strenuous physical activity may not be advisable for people with advanced heart failure, regular, moderate exercise can strengthen the heart, improve circulation, and reduce symptoms. A supervised cardiac rehabilitation program may be recommended to ensure safe and effective exercise.
- Weight The board: Keeping a solid weight is significant for overseeing CHF. Being overweight puts additional strain on the heart, while sudden weight gain can indicate worsening heart failure due to fluid retention.
- Quit Smoking: Smoking damages blood vessels, reduces oxygen levels in the blood, and worsens heart failure. Quitting smoking is one of the most effective steps you can take to improve heart health and prevent further complications.
- Alcohol Reduction: Excessive alcohol can weaken the heart muscle and worsen heart failure symptoms. Your doctor may recommend limiting alcohol or avoiding it altogether.
- Manage Stress: Chronic stress and anxiety can increase blood pressure and strain the heart. Incorporating relaxation techniques, such as deep breathing, meditation, or yoga, can be beneficial for heart failure patients.
3. Medical Devices
For individuals with more severe congestive heart failure, certain medical devices may be used to help the heart function more effectively:
- Implantable Cardioverter-Defibrillator (ICD): An ICD is a small device implanted in the chest to monitor the heart’s rhythm. If it detects a dangerous arrhythmia, it delivers a shock to restore normal heart rhythm.
- Cardiac Resynchronization Therapy (CRT): This therapy uses a special pacemaker to coordinate the contractions of the heart’s ventricles, improving heart function. CRT is often recommended for patients with severe heart failure and an abnormal heart rhythm.
- Ventricular Assist Devices (VADs): VADs are mechanical pumps that help the heart pump blood more effectively. They are often used as a temporary solution while a patient waits for a heart transplant or as a long-term treatment for people who are not candidates for transplantation.
4. Surgical Options
In some cases, surgery may be required to treat the underlying cause of congestive heart failure or to improve heart function:
- Coronary Artery Bypass Surgery: For patients with heart failure caused by blocked arteries, coronary artery bypass surgery can improve blood flow to the heart muscle by bypassing blocked coronary arteries.
- Heart Valve Repair or Replacement: If heart valve disease is contributing to heart failure, surgery may be required to repair or replace the faulty valve to improve heart function.
- Heart Transplant: In cases of end-stage heart failure where other treatments are no longer effective, a heart transplant may be the only option. This procedure replaces the damaged heart with a healthy donor heart.
5. Monitoring and Regular Check-Ups
Congestive heart failure is a chronic condition that requires ongoing monitoring. Regular check-ups with your cardiologist and other healthcare providers are essential to managing the condition. This may include:
- Home Monitoring: Monitoring your weight daily and reporting any sudden increases to your doctor can help catch early signs of fluid retention. Additionally, monitoring your blood pressure and heart rate can provide valuable information about how well your heart is functioning.
- Follow-Up Tests: Periodic tests, such as echocardiograms, stress tests, and blood tests, may be conducted to assess your heart’s condition and adjust your treatment plan as needed.
Complications of Congestive Heart Failure
Without proper management, congestive heart failure can lead to serious complications that further affect a person’s quality of life and increase the risk of mortality. Probably the most well-known complexities include:
- Kidney Damage: CHF can reduce blood flow to the kidneys, leading to kidney damage or even kidney failure. Managing heart failure and protecting kidney function often go hand-in-hand.
- Liver Damage: Fluid buildup in the liver can lead to scarring, inflammation, and liver damage over time.
- Arrhythmias: Heart failure increases the risk of abnormal heart rhythms, which can lead to stroke or sudden cardiac arrest.
- Heart Attack and Stroke: CHF increases the risk of developing blood clots, which can cause heart attacks or strokes.
- Pulmonary Hypertension: The increased pressure in the blood vessels in the lungs due to left-sided heart failure can lead to pulmonary hypertension, further worsening the condition.
Preventing Congestive Heart Failure
While not all cases of congestive heart failure can be prevented, many risk factors are manageable through lifestyle changes and medical intervention. Here are some preventive measures that can reduce the risk of developing heart failure:
- Control High Blood Pressure: Managing hypertension through diet, exercise, and medication is essential for reducing the strain on the heart.
- Manage Diabetes: Keeping blood sugar levels under control through proper medication, diet, and exercise can significantly reduce the risk of heart failure in people with diabetes.
- Reduce Cholesterol Levels: Lowering LDL cholesterol through dietary changes, exercise, and medication can help prevent coronary artery disease, a leading cause of heart failure.
- Limit Alcohol and Quit Smoking: Both smoking and excessive alcohol consumption increase the risk of heart failure. Quitting smoking and reducing alcohol intake are key steps in heart failure prevention.
- Maintain a Healthy Weight: Obesity is a major risk factor for heart disease and heart failure. Keeping a sound load through diet and exercise can diminish your gamble.
- Regular Check-Ups: If you have a family history of heart disease or other risk factors, regular check-ups with your healthcare provider can help detect early signs of heart problems and take preventive measures.
Conclusion
Congestive heart failure is a chronic and serious condition that requires careful management. While there is no cure for congestive heart failure, early diagnosis, lifestyle changes, medications, and in some cases, surgery, can significantly improve quality of life and reduce the risk of complications. Understanding the symptoms, causes, and treatment options for congestive heart failure is essential for anyone at risk of developing the condition, as well as for those already living with it.
If you or someone you know is experiencing symptoms of congestive heart failure, it’s important to seek medical attention promptly. Early intervention and comprehensive treatment can help manage the condition, prevent worsening symptoms, and extend life expectancy. By making lifestyle adjustments and adhering to prescribed treatments, it’s possible to live a full and active life, even with congestive heart failure.
FAQs
What is the difference between congestive heart failure and heart attack?
A heart attack occurs when blood flow to a part of the heart is blocked, causing damage to heart tissue. Congestive heart failure, on the other hand, is a chronic condition where the heart becomes weak and unable to pump blood efficiently, leading to fluid buildup in the body. A heart attack can contribute to heart failure, but they are distinct conditions.
Can congestive heart failure be reversed?
Congestive heart failure is a chronic condition and, unfortunately, cannot be cured or fully reversed. However, with proper treatment, lifestyle changes, and medication, it is possible to manage the symptoms, improve heart function, and prevent further damage.
What are the early warning signs of congestive heart failure?
Early signs of congestive heart failure include shortness of breath, especially during physical activity, fatigue, swelling in the ankles, legs, or feet (edema), and frequent coughing or wheezing. Early detection can help manage the condition more effectively.
How is congestive heart failure diagnosed?
Congestive heart failure is diagnosed using a combination of methods including a physical exam, echocardiogram (to assess heart function), electrocardiogram (ECG), chest X-ray, and blood tests to look for signs of heart failure, such as elevated B-type natriuretic peptide (BNP) levels.
What lifestyle changes can help manage congestive heart failure?
Key lifestyle changes include following a low-sodium, heart-healthy diet, maintaining a healthy weight, engaging in regular moderate exercise, quitting smoking, limiting alcohol intake, managing stress, and closely monitoring fluid intake. These changes can significantly improve quality of life and reduce the risk of complications.